Weaknesses in EMS Patients
Particular Kinds of Neuromuscular Diseases
Nerves that regulate voluntary muscles and nerves that relay sensory data to the brain are both impacted by neuromuscular diseases. To help control voluntary muscles, nerve cells, or neurons, transmit and receive electrical signals to and from the body. Communication between the nervous system and muscles is disrupted when neurons deteriorate or die. Muscles deteriorate and weaken as a result (atrophy).
Symptoms
Many neuromuscular problems exist, and it is crucial that they are treated by a skilled multidisciplinary team, like the one at Cedars-Neuromuscular Sinai’s Disorders Department.
Muscle weakness and weariness brought on by these illnesses worsen over time. While the symptoms of some neuromuscular illnesses first manifest in children, those of others might develop as children or even adults.

Unilateral Weakness
combination of ipsilateral face involvement and an arm, hand, or leg
A lesion in the contralateral cerebral cortex or the CSTs running down the corona radiata and forming the internal capsule is typically to blame for weakness involving the combination of an arm, hand, or leg with ipsilateral facial involvement. Moderate variants are typically characterized by a decline in hand dexterity and coordination. Paresis refers to a moderate loss of strength, while plegia refers to a total lack of motion. Although UMN symptoms are helpful corroborations, they are not always present, particularly in the acute phase. Over the weak areas, sensory disruptions are frequent. To localize the problem, look for neglect, visual field loss, or expressive or receptive aphasia the problem to the cortex.
Patients who experience equal weakness in their face, hand, and leg are more prone to suffer from a subcortical lesion that disrupts all of these fibres as they bundle up in the internal capsule. Even though complicated migraines might result in focal neurologic impairments, a concurrent headache raises the possibility of a mass lesion or brain haemorrhage. Acute ischemia or haemorrhage is frequently suspected when this weakening pattern develops suddenly, although demyelination (such as multiple sclerosis or severe demyelinating encephalomyelitis) or tumours may present gradually.
Combination of the contralateral face region and an involved arm, hand, or leg
A brainstem lesion is indicated by weakness in the arm, hand, or leg when the opposing face muscles are also affected. Further information may be revealed by a thorough CN analysis. Ptosis is probably present if the patient displays contralateral facial abnormalities (CN III or sympathetic fibres) or a forehead-involved facial droop (CN VII nucleus). The malfunctioning of CN V, VI, VIII, IX, or XII will help localize to a specific level in the brainstem. On examination, there may also be cerebellar findings or nystagmus. Weakness can be accompanied by sensory problems, and some patients may have double vision, feel sick, difficulty speaking dizziness, or vomiting and nausea.
Combination of the arm, hand, or leg without the use of the face
Without face involvement, weakness involving an arm, hand, or leg is most likely caused by one of the following three processes:
• A distinct internal capsule or brainstem lesion affecting solely the corticospinal pathways rather than the corticobulbar tracts, over the region where the lower extremity is represented.
• If the patient additionally has contralateral hemibody discomfort and temperature sensory alterations below the level of motor weakness, a brainstem lesion or a Brown-Séquard internal capsule may be present.
But before a patient is put in this category, it’s crucial to carefully assess facial symmetry to make sure there isn’t any nasolabial fold effacement or slight facial droop.
Isolated weakness in an extremity (mono paresis or monoplegia)
A spinal cord or peripheral nerve injury is typically the source of isolated weakness in one extremity. Finding uncommon monomeric presentations of CNS lesions will be made easier by looking for UMN symptoms in the affected limb.
A comprehensive evaluation is done for facial weakness or involvement of the contralateral or other ipsilateral limbs as symptomatic of a central process if UMN indications like hyperreflexia or spasticity are present.
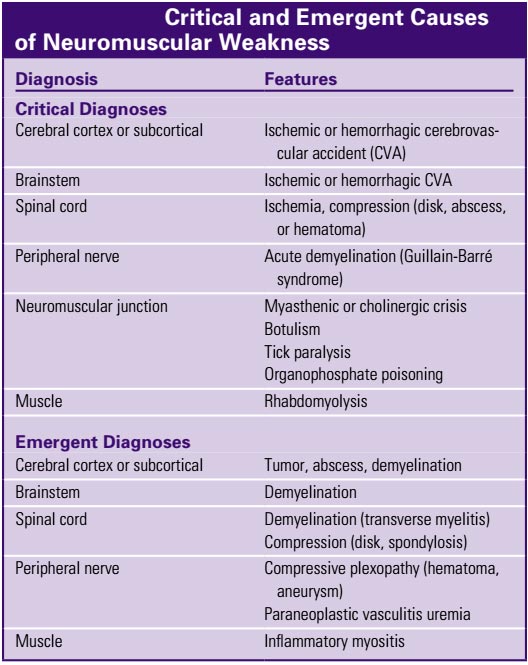
Be that the patient does not have a contralateral pinprick level suggestive of Brown-Séquard hemicord syndrome if they only have weakness in one lower limb entirely. Radiculopathy, plexopathy, peripheral neuropathy, or NMJ disease frequently cause monomeric weakness. For urgent and crucial PNS diagnosis see the below picture.
Bilateral Weakness
only the lower extremities (paraparesis or paraplegia)
The first thing to investigate when weakness mainly affects the lower extremities is spinal cord damage.
If this is the case, the acute phase may not exhibit UMN indications.
Patients with bilateral lower extremity paralysis frequently experience changes in their feeling of pain or temperature since the lateral spinothalamic tracts (LSTs) are located close to the CST.
The patient may develop peripheral neuropathy that affects the longest nerve tracts first if a cord condition or cauda equina compression is not indicated by the physical examination.
Guillain-Barré syndrome is the acute manifestation that is most worrying (GBS). Asymmetrical weakness that rises from the foot can be caused by the rapid demyelination of peripheral nerves.
Only the Upper Body
The corticospinal fibres responsible for hand and arm strength are located in the middle region of the cervical spinal cord, where weakening solely affects the upper extremities. Because of the involvement of crossed sensory axons heading for the contralateral LST, the patient may suffer pinprick sensation loss over the upper limbs. Nonetheless, the posterior columns should continue to play a role in mediating mild touch sensation.
Syringomyelia and injuries to the cervical spine’s hyperextension are frequent causes of central cord syndrome.
Without facial involvement, all four extremities (quadriparesis or quadriplegia)
The main worry is cervical spinal cord damage or process when weakness affects all four extremities without including the face, however, the patient is first examined for illnesses that cause generalized weakness. The likelihood that the patient has an issue with the cervical spinal cord increases with the density of the extremities’ weakness. Quadriparesis typically exhibits considerable disparity between the lower and upper limbs, despite the fact that all four extremities will test poorly for muscle strength.
Localization of the level within the cervical spinal cord will be possible by the use of pinprick testing to identify sensory dermatomes in the hands and arms as well as strength testing of particular myotomes. Because anterior cells are involved at this specific level, upper extremity myotomes corresponding to the region of spine involvement will actually exhibit LMN indications of flaccid weakness and reduced reflexes in conditions that induce cord compression or ischemia. Nonetheless, below that threshold, UMN indications might be evoked. For instance, a C5 lesion can result in weaker biceps reflexes but stronger triceps and patellar responses.
Patients with GBS that have progressed from the upper extremity peripheral nerve myelin sheaths to the lower extremities may experience bilateral extremity weakness. The lower limbs are typically weaker than the upper limbs in this situation.
External restraint (entrapment syndrome, compressive plexopathy) Endocrinopathy (diabetes) (diabetes)
The paraneoplastic disorders
Toxins (alcohol) (alcohol)
Trauma
vitamin shortage
DISPOSITION
Individuals with generalized weakness should be treated and managed according to the underlying illness and expected therapeutic course; the range of attitudes will change according to the cause. Individuals with thrombotic or hemorrhagic central vascular lesions should get rigorous inpatient management. If it is believed that a patient’s benign myofiber weakness or moderate LMN is not expected to worsen quickly, the patient may be discharged with strict monitoring. Any patient with new UMN weakness and those with more severe or worsening LMN or myofiber weakness should be hospitalized for additional testing. Individuals who may have ascending paralysis should be hospitalized in an intensive care unit (ICU) for close respiratory monitoring.