Airway Care
The foundation of resuscitation is airway management in emergencies, which also serves as a defining competency for the field of emergency medicine. All emergency airway procedures fall under the purview of emergency medicine, and the emergency physician is primarily responsible for airway management.
Physiology, Pathophysiology, and Anatomy
The selection to intubate is based on a careful evaluation of the patient and the clinical presentation according to three crucial criteria:
- Failing to protect or sustain the airway
- Inadequate oxygenation or ventilation
- The expected clinical course and the likelihood of worsening for the patient

KEY CONCEPTS in Airway management in emergencies
- The physicians must consider the clinical patient’s state and the possibility of failing when choosing to intubate. In particular, if the patient leaves the emergency department (ED) for a while.
- Before using a neuromuscular blocking agent (NMBA), the emergency team evaluates a patient for some problems such as difficult intubation, bag-mask ventilation (BMV), ventilation using an extragalactic device (EGD), and cricothyrotomy.
- This is true even though video laryngoscopy (VL) has decreased the likelihood of a failed intubation try caused by difficult anatomic features that frequently prevent direct laryngoscopy (DL).
Physiologic dysregulation
- Physiologic dysregulation during emergency airway care can increase the risk of morbidity and fatality. When time permits, the doctor should perform cardiovascular optimization to lower the risk of circulatory collapse and cardiac arrest using fluids, blood, and pressure agents.
- Rapid sequence intubation (RSI) is the airway management in emergencies for emergency department patients when airway care is not problematic.
- After intubation, it is crucial to confirm the tube’s location using end-tidal carbon dioxide (ETco2).
- If the emergency team cannot detect sufficient amounts of exhaled CO2, use oesophagal intubation unless disproven otherwise. Even when they use DL concerning different optimization strategies, VL improves first-attempt intubation success.
First-attempt success (FAS)
- First-attempt success (FAS) relates to greater results and fewer negative side effects.
- Emergency airway managers should become familiar with and use VL as their go-to emergency intubation technique.
- Once the failed airway scenario known as “can’t intubate, can’t oxygenate” has been diagnosed, cricothyrotomy is indicated. Delays could enhance the patient’s risk or severity of hypoxia harm.
The process of RSI
- More than 90% of all RSIs use etomidate.
Succinylcholine or rocuronium are appropriate NMBAs to utilize during RSI. - Although its activity lasts longer with rocuronium, it has a lower risk of side effects.
- Paramedics use EGDs infrequently in ED airway care. In spite the fact that they are widely used in prehospital systems and provide additional choices for oxygenation rescue in failing airways.

Failing to protect or maintain the Airway
An open airway is crucial for adequate ventilation and natural action. If a patient is unable to take care of an open airway, ought to establish by victimization airway management steps. Such as location, chin lift, jaw thrust, or insertion of an associate oral or nasal airway. Likewise, the patient should be ready to shield against the aspiration of internal organ contents. It carries vital risks for morbidity and mortality. traditionally, the presence of a physiological reaction has been advocated as a reliable indicator of the patient’s ability to guard the airway. However, this has been definitively evidenced to be unreliable as a result of the physiological reaction being absent in the 12-tone system the twenty-fifth of traditional adults. There’s no proof that its presence or absence corresponds to airway-protecting reflexes or predicts the requirement for canulization. The patient’s ability to swallow or handle secretions may be an additional reliable indicator of airway protection.
An Approach to Gauging the Patient’s Level of Consciousness
The suggested approach is to gauge the patient’s level of consciousness. Its ability to vocalize in response to voice command or query, that provides info regarding the integrity of the higher airway and level of consciousness; and skill to manage their own secretions. For example, the pooling of secretions within the bodily cavity, and lack of swallowing.
In most cases, clinical assessment, together with pulse oximetry with or while not capnography, thought of the timeline of the patient’s metabolism emergency, and observation of improvement or deterioration within the patient’s clinical condition can cause an accurate call.
Failing to Ventilation or Oxygenation
Gas exchange, including oxygenation and carbon dioxide elimination, is necessary for the proper operation of essential organs. A key indication for intubation is chronic hypoxemia despite maximal oxygen supply or ventilator failure that is not readily reversible. The patient’s general condition, oxygen saturation measures by pulse oximetry and ventilatory pattern are all evaluated as part of this clinical assessment. If oximetry results are accurate, continuous capnography is another option that may be useful but is not necessary. ABGs are essential to determine whether we need to intubate a patient or a practical way to obtain them before emergency intubation. ABGs may also be deceptive, resulting in a false sense of security. This causes delaying the intubation of a patient who is deteriorating.
While fast asthma, for instance, may need intubation even though ABG values are only mildly disrupted, patients who are clinically improving despite severe or seemingly worsening ABG abnormalities may not need it.
Phyisicians will make a correct choice typically based on clinical assessment, which may include pulse oximetry with or without capnography, consideration of the patient’s timetable for their respiratory emergency, and monitoring of improvement or deterioration in their clinical status.
Managing airways in emergencies can be difficult
Intubation is a simple process for the majority of patients in terms of airway control in emergencies. Although ED-based observational registries previously estimated cricothyrotomy rates for all intubations to be approximately 1%, a more recent study has discovered a lower prevalence of less than 0.5%.
As would be expected with an unselected, unplanned patient population, the rate of cricothyrotomy in the emergency room, where it occurs is roughly 1 in 200 to 2000 elective general anesthetic events. Bag-mask ventilation (BMV) is difficult for roughly 1 in 50 patients under general anesthesia and impossible for about 1 in 600 individuals.

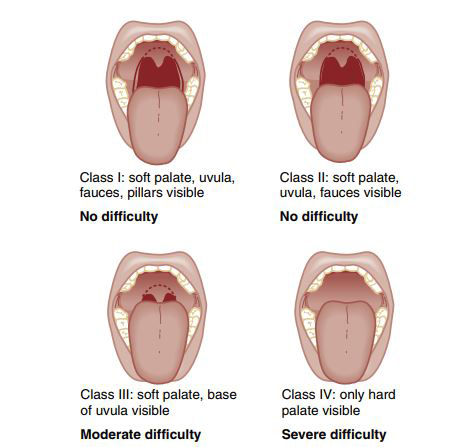
The populations of ED patients who are critically ill or injured and for whom intubation is urgent and necessary does not estimate from these data. A preintubation examination of characteristics predicting difficult intubation provides the clinician with the knowledge necessary to develop a safe and effective intubation plan. The doctor examines the patient before intubation. This looks for anatomical characteristics. It might indicate a difficult airway. This comprises BMV, placement of and ventilation with an extraglottic device (EGD) and a potential problem with laryngoscopy and intubation. To successfully plan, it is essential to know all four areas. The emergency clinician should always prepare for a difficult-to-manage airway.
The Spectrum of Airway care
Airway care issue exists on a spectrum. Some patients have one minor anatomic or pathophysiologic reason for airway management issues. Whereas patients who have different airway characteristics complicate laryngoscopy, bag ventilation, use of associate EGD, and cricothyrotomy. The second group, in particular, if obstructing higher airway pathology is part of the problem, has crossed a threshold of obstacles beyond which neuromuscular clog would avoid. It would result in a “can’t intubate, can’t oxygenate” (CI: CO) failing airway may result.
In these cases, the famous approach is to use an anaesthesia method, with titrated sedation, to gain intubation without using a neuromuscular blocking agent (NBMA). When intubation is undertaken with standard laryngoscopy or using NBMAs causes immediate physical damage, patients with refractory hypoxemia or extreme metabolic acidosis may be intolerant to brief periods of apnea.
It is important to understand the state of consciousness of a patient. Since it helps in providing proper care. This is where having an AI tool that can gauge the level of consciousness can be helpful. Surec app is an intelligent assistant which helps paramedics speed the process of rescuing a patient at an incident scene.